What can you measure to find out whether dysphagia therapy is on track?
True Angle is serious about getting the Mobili-T system into the hands of clinicians looking to level up their swallowing therapy. Giving patients access to all the tools they need in order to take charge of their swallowing rehabilitation is what keeps us going.
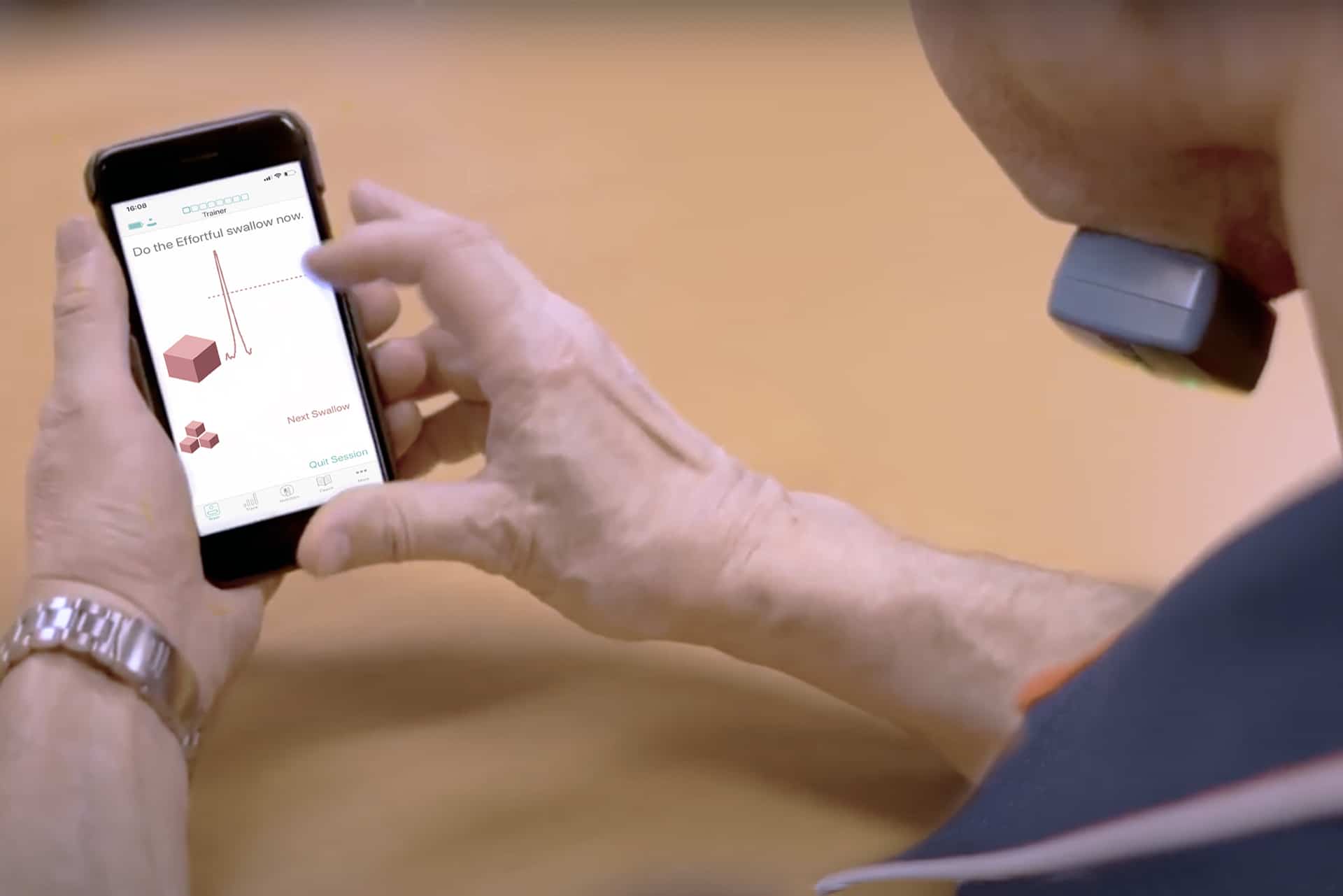
Mobili-T is a system made up of a device, an app, and a clinician portal. The device sticks under the chin and uses surface electromyography (sEMG) sensors to detect the activity of the swallowing muscles under your chin. This information is instantly translated onscreen in the iOS app and is shown to you as biofeedback.
So with all this beautiful biofeedback, a common question we get asked is: “How strong should the swallow be?” or “Does Mobili-T provide measurements for amplitude?”
Essentially, you may be wondering if you should care about how high that line goes up and if it translates into some nice numbers for your quantitative data. S-LPs love data because it helps us track progress. No one can deny the persuasive quality of changing numbers.
The short answer to those questions is no. Let’s have a look at why.
(Fear not! Measurements will come!)
Quantitative Data & Swallowing Strength
Is sEMG helpful to give us quantitative data on swallowing strength?
sEMG is measured in microvolts (µV), represented on the screen as amplitude. More µV indicates stronger muscle excitation, which could be related to stronger muscle contraction, but not always. The number cannot reliably measure function because there are too many variables. Amplitude expressed in µV can vary swallow to swallow and day to day based on:
- Placement of device: slightly different placement means the signal may be resulting from excitation of more/less or bigger/smaller muscle fibers on any given session
- Presence of submental fat or swelling: this may interfere with the signal strength
- Types of bolus used: different textures, tastes and temperatures can affect how a swallow is triggered and how the muscles are engaged
- How a device interprets raw signal: each sEMG technology out there has their own methods to ensure the signal you care about is clear and easy to understand. Comparing sEMG amplitudes from different devices just isn’t informative in this case.
The amplitude is raw data that cannot be interpreted on its own. It does not tell us:
- What is a “normal” swallow for that person
- If there is impairment at another level – a person could have a strong swallow, but still be aspirating or still need more fluids to wash it down
- If more muscle excitation is translating into better function
Muscle excitation as interpreted by sEMG just shows us muscle excitation, not actual function.
Even if we could control for all the variables, a stronger swallow does not mean a more functional swallow. If the goal of treatment is better function, measuring amplitude means we could be missing the mark.
To truly understand function, we still have to engage our assessment tools like Modified Barium Swallowing Studies (MBSS) or fiberoptic endoscopic evaluation of swallowing (FEES).
Then what are we measuring?!
How Does Visual Feedback Help Understand Swallow Strength?
If we get back to the root of what sEMG can provide, it’s that visual biofeedback.
The visual helps people understand, become aware and engage in swallowing exercises. sEMG can be your coach to help train patients towards doing better on functional evaluations, or the everyday task of enjoying a favorite food again.
Mobili-T provides easy access to that sEMG “coach” that we previously couldn’t find in what was available.
When patients have access to their swallowing exercise motivator or coach at home, multiple times daily or just hanging out in their pocket, there are lots of successes we can measure:
- The ability to complete a swallowing exercise (did they do that effortful swallow…or did they just say/think they did an effortful swallow?)
- Number of successfully completed repetitions of a swallowing exercise
- Number of days engaged in a swallowing exercise routine
What sEMG and Mobili-T allow you to track is patient understanding, engagement, and adherence to their swallowing exercise workouts. When patients are not experiencing any functional changes, you can get to the root of why that may be. This may mean reteaching some exercises if that line is consistently not hitting the target, or being able to give accurate feedback as to if the recommended dosage is being completed. Isn’t it nice to have data to help you make decisions?
While we won’t be using Mobili-T to test muscle strength (we’re using it to visualize muscle excitation!), we use it to allow clinicians and patients to take some of the guesswork out of therapy and see the goals they can actually reach. That’s what we call empowering.