How SLPs can leverage technology for better patient outcomes and better business
You may be hearing buzz from your OT and PT colleagues about how they are able to use Remote Therapeutic Monitoring (RTM) codes. RTM codes were created in 2022 to give therapists (OTs, PTs, SLPs) a way to extend musculoskeletal (MSK) treatments (think dysphagia therapy) outside the clinic. If you’re thinking, “I already do that with my patients’ home programming!”, the difference is that RTM codes allow you to bill for it. Doing the work AND getting recognized?! Count us in.
While SLPs are included as RTM providers, something is missing from our toolkits. Remote monitoring requires specific technology you can use to connect with your patient once they go home. What exactly are you sending home with your patients that allows you to monitor them remotely?
Let us walk you through more about how SLPs can get in on RTM services and how their patients and businesses can benefit.
What are the Advantages of Remote Therapeutic Monitoring Services for SLPs and Dysphagia Therapy?
Before we get into the details as to what RTM is and how SLPs can provide remote monitoring, let’s talk more about why it applies.
With a rapidly changing and more technology-focused world, people have come to expect that they should be able to accomplish tasks remotely. Remote therapy services are an increasing trend and dysphagia therapy is innovating to keep up.
These are some of the advantages of using RTM.
1. Get patients more engaged in therapy
Access to clinical tools at home improves adherence and engagement. In a survey done by Medbridge, patients increased their activation in therapy by over 80% when RTM was incorporated1. Having tools that can be monitored by a clinician to give feedback and personalize programming ensures patients are truly getting what they need.
2. Provide convenient and better access to care
All too often patients disengage from therapy due to access.
RTM services ensure patients who cannot regularly visit a clinic can still have an informative, two-way relationship with their clinician. In addition to being more convenient, this means patients with mobility issues or those in more remote areas can still access treatment.
3. Better outcomes
More engagement and better access to care means patients are more likely to see the maximum benefits of therapy. Research shows that swallowing exercises are rarely completed as well or as frequently as is prescribed2.
How can we expect patients to improve if they don’t have the tools and communication with their SLP to stay on top of their program?
4. Generate revenue through use of RTM CPT codes
Even if you aren’t a business owner, this hits home with many of the higher-ups, showing the value of SLPs’ work.
Gain the ability to account for the time spent following up with patients at home. The use of RTM codes ensures the work clinicians are doing is recognized both in time and financially.
If you’re curious as to how an RTM-qualifying device like Mobili-T can add additional revenue, try our RTM calculator.
What is Remote Therapeutic Monitoring (RTM)?
Remote Therapeutic Monitoring codes were introduced in 2022 to enable providers to oversee therapy remotely AND get reimbursed for those services. We all know SLPs are already putting in time following up with patients outside the clinic. Let’s find a way to get that work recognized on the books! These include monitoring and collecting non-physiological data, such as therapy and response to treatment, from patients via an approved medical device.
ASHA describes each RTM CPT code that may apply to SLPs in detail.
It should be noted that RTM is not the same as teletherapy. RTM means the patient is doing most of the work on their own time with information about their activity and performance available remotely to their clinician. Follow-ups are completed via call or video but this is to check-in on the patient’s progress, not to complete every therapy session with them in real-time.
What do you need to provide Remote Therapeutic Monitoring services for dysphagia?
- The ability to collect and monitor non-physiologic patient therapy data remotely via software or app
- A device that meets the standard set forth by the FDA as a medical device
How does RTM apply to SLPs working with dysphagia?
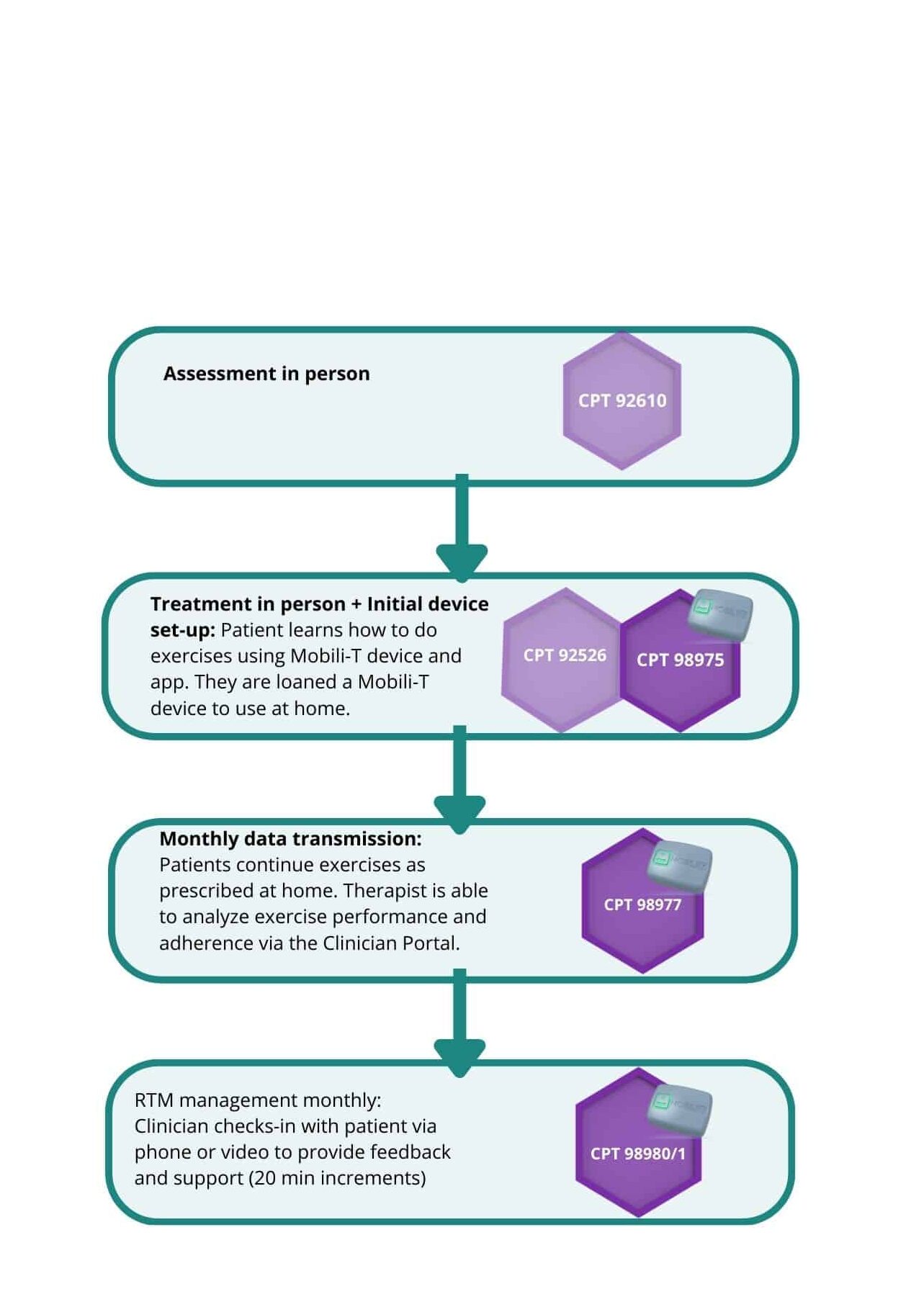
Dysphagia patients are often sent home with an exercise program. Many SLPs are already checking in with their patients and their home programs outside the clinic, and RTM codes make these eligible for reimbursement. The standard check in of, “Did you do your exercises as prescribed?” from their SLP doesn’t qualify as RTM. You need to be able to monitor the musculoskeletal (MSK) system related to swallowing somehow.
Monitoring therapy adherence (are patients doing the exercises?) and response to therapy (are they achieving the targets set out in therapeutic exercises?) while patients complete their therapy at home would make their home workouts eligible for RTM.
What does this look like in action?
Mobili-T is a small, wearable device that was designed to provide biofeedback on the MSK system during swallowing. Using the Mobili-T device and accompanying app, you can “see” the swallow through the science of surface electromyography (sEMG). Clinicians can then access a patient’s performance and modify their programming via Mobili-T’s Clinician Portal Software.
Using Mobili-T to monitor adherence and performance with dysphagia exercises, the following CPT codes could be used:
Patients everywhere have discovered the convenience and advantage to being able to continue their journey to health from the comfort of home. There is no reason dysphagia therapy should be left out. We’re here to help you Level-up care, stay on top of the latest technology and provide evidence-based dysphagia therapy.
Want more information on the clinical pathway for billing RTM services? Download our Therapeutic Billing Pathway here or contact us to get started on implementing RTM services with Mobili-T
References:
- Medbridge, Boosting Patient Activation in Older Adults with Digital Healthcare Technology. https://www.medbridge.com/enterprise/resources/boosting-patient-activation-in-older-adults-with-digital-healthcare-technology/
- Choy J, Pourkazemi F, Anderson C, Bogaardt H. Dosages of Swallowing Exercises Prescribed in Stroke Rehabilitation: A Medical Record Audit. Dysphagia. 2022 Aug 11. doi: 10.1007/s00455-022-10500-x. Epub ahead of print. PMID: 35951119.