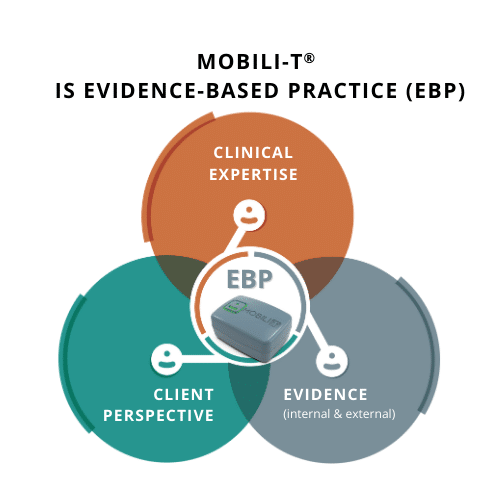
Clinicians are dedicated to ensuring the treatment they provide to patients is the best available. While evidence-based solutions are often equated to being backed by quality research, it is also the integration of the three aspects of evidence-based practice (evidence-based practice) that have guided the development of Mobili-T as an evidence-based, dysphagia therapy tool.
Since its initial design, we have been consistently modifying Mobili-T to better suit clinician and patient needs. We are proud to be providing a tool to clinicians that we can firmly say is based on and contributes to evidence-based practice.
Read on to find out how by providing convenient access to sEMG biofeedback for swallowing exercises, Mobili-T is pushing evidence-based dysphagia rehab tools into the future.
1. Evidence (External and Internal)
External Evidence (from scientific literature)
This is an area where Mobili-T shines. The system incorporates techniques from the best research available on motor learning, exercise and dysphagia.
- The Principles of Motor Learning are evidence-based
Mobili-T’s exercises are based on the principles of motor learning which facilitate retention of new motor skills. Part of this is that in order to see improvement in a specific motor pattern, we need to work on that pattern. In the case of dysphagia, if we want to see improvement in the swallow, we need to work on the swallow.1 - Therapeutic exercises for dysphagia rehabilitation are evidence-based
Studies show that taking part in a swallowing exercise program can reduce length of hospital stays, decrease incidence of chest infections and result in faster return and improved oral intake2-4.
- The importance of exercise adherence for positive outcomes is evidence-based
Research shows that it does matter how many repetitions and how often swallowing exercises are performed. Without a reliable tracking method, swallowing exercises are typically not completed with the intensity and frequency as prescribed. What patients are doing is not clinically optimal!5 For example, with an effortful swallow, they may not be hitting their target for effort, or doing enough repetitions to reach the exercise’s full effect. The evidence shows if we could be teaching dysphagia exercises with more precision and helping patients adhere to the optimal dose, this leads to better functional results5-7.
- The positive impact of surface electromyography (sEMG) biofeedback used with dysphagia exercises to improve adherence is evidence-based
Pairing sEMG with dysphagia rehabilitation exercises has been shown in several studies to result in improved swallowing outcomes when compared to dysphagia exercises alone6. In a Mobili-T-specific study, use of sEMG biofeedback maintained high adherence to exercise programs over a 6 week period.8
Internal evidence (from data and observations specific to the patient):
Data and observations of a particular patient are key pieces of evidence that clinicians consider during treatment. With most current ways of completing swallowing exercises, the clinician relies on patient reports: Did you complete your exercises? How many? Did you hit your targets?
That’s why we designed Mobili-T to give you the patient data you need to make more informed clinical decisions.
With the Mobili-T sensor and the app, you can get immediate evidence that your patient completed a repetition of their exercise by seeing the biofeedback line appear in the app. With the addition of the Clinician Portal for exercise customization and monitoring, you can keep track of their adherence to targets and repetitions remotely.
This need for internal evidence to guide treatment has been one of the benefits of using technology as part of dysphagia exercises. Director of Stanford’s Head and Neck Cancer Speech and Swallowing Rehabilitation, Heather Starmer, points this out saying, “[Mobili-T] gives us the data points to have realistic conversations about expectations with patients. If you’re not doing what’s recommended, that’s probably going to contribute to why you’re not changing. So I think it helps on both ends. It helps the patients do better quicker, but it also helps us to rope them back into reality if we need to.”
She also notes that the internal evidence is helpful when shaping programs or advocating for therapy tools. “The nice thing is that because we’ve got all that information within the Clinician Portal, if I needed to, I could very easily pull it and say, of the last 10 people that I’ve given this to, here’s the level of engagement, here are the outcomes that we’ve been able to accomplish.”
Now, that’s some pretty convincing evidence.
2. Clinical Expertise
We believe in equipping our clinicians with the tools they need to become proficient users of new technology. Training and orientation to Mobili-T does not require a special certification. Everything you need to know is included. We also provide you with resources such as webinars and a Resource Hub to keep your clinical expertise up to date.
Ensuring a supportive experience with Mobili-T has been a priority for our team and has shaped the way we help new users incorporate it into their practice.
One inpatient hospital team told us:
“We found it very supportive that the team would provide us with really well thought out answers, pulling in the evidence that they were aware of and providing suggestions. From the education and support piece, it was something that we haven’t had with any kind of technology that we’ve purchased.”
The last thing any facility needs is underutilized technology, so as a tool developed by clinicians, we use our years of clinical expertise in dysphagia to contribute to your continuing expertise.
3. Client Perspectives
As we discussed above, we have the external evidence to show that biofeedback can help motivate patients. External evidence even points towards sEMG contributing to positive therapy experiences for patients.7 While Mobili-T was developed with much consideration for the patient experience, actual use has validated what we set out to do.
Feedback we’ve received from Mobili-T users contain themes of feeling motivation, empowerment and effectiveness:
“I made more gains in the six weeks wearing the device and going through that process than I did at any time prior, in terms of my swallowing.”
–David J. Mobili-T User
“I was using the device through my clinician at Stanford but had to turn it in. I loved it so much, I purchased one for myself. I have moved from just water to having one meal a day.”
-Mobili-T user
Giving patients a more positive, hopeful and rewarding experience with their rehabilitation journey is fundamental to evidence-based practice.
Clinicians are looking for evidence-based solutions. In today’s growing technology world, dysphagia rehabilitation shouldn’t get left behind. This is why the components of evidence-based practice have guided the development of Mobili-T to make technology affordable and accessible, in order to bring tools for swallowing therapy into the future.
References
- Huckabee, M. L., & Macrae, P. (2014). Rethinking rehab: Skill-based training for swallowing impairment. SIG 13 Perspectives on Swallowing and Swallowing Disorders. Dysphagia, 23(1), 46-53. https://doi.org/10.1044/sasd23.1.46
- Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018 Oct 30;10(10):CD000323. Doi: 10.1002/14651858.CD000323.pub3. PMID: 30376602; PMCID: PMC6516809.
- Gillman A, Hayes M, Sheaf G, Walshe M, Reynolds JV, Regan J. Exercise-based dysphagia rehabilitation for adults with oesophageal cancer: a systematic review. BMC Cancer. 2022 Jan 10;22(1):53. Doi: 10.1186/s12885-021-09155-y. PMID: 35012495; PMCID: PMC8751332.
- Jongprasitkul, H., & Kitisomprayoonkul, W. (2020). Effectiveness of Conventional Swallowing Therapy in Acute Stroke Patients with Dysphagia. Rehabilitation Research and Practice, 2020.
- Choy J, Pourkazemi F, Anderson C, Bogaardt H. Dosages of Swallowing Exercises Prescribed in Stroke Rehabilitation: A Medical Record Audit. Dysphagia. 2022 Aug 11. doi: 10.1007/s00455-022-10500-x. Epub ahead of print. PMID: 35951119.
- Albuquerque LCA, Pernambuco L, da Silva CM, Chateaubriand MM, da Silva HJ. Effects of electromyographic biofeedback as an adjunctive therapy in the treatment of swallowing disorders: a systematic review of the literature. Eur Arch Otorhinolaryngol. 2019 Apr;276(4):927-938. Doi: 10.1007/s00405-019-05336-5. Epub 2019 Feb 15. PMID: 30771061.
- Archer SK, Smith CH, Newham DJ. Surface Electromyographic Biofeedback and the Effortful Swallow Exercise for Stroke-Related Dysphagia and in Healthy Ageing. Dysphagia. 2021 Apr;36(2):281-292. Doi: 10.1007/s00455-020-10129-8. Epub 2020 May 22. PMID: 32445060; PMCID: PMC8004490.
- Constantinescu G, Rieger J, Seikaly H, Eurich D. Adherence to Home-Based Swallowing Therapy Using a Mobile System in Head and Neck Cancer Survivors. Am J Speech Lang Pathol. 2021 Nov 4;30(6):2465-2475. Doi: 10.1044/2021_AJSLP-21-00026. Epub 2021 Aug 31. PMID: 34463544.