How one SLP used the Mobili-T® system to restore her patient’s swallow and quality of life
What would you do if you had a patient with a 30 year history of dysphagia due to a congenital neuromuscular disorder? This was what one of our Mobili-T clinicians found on her caseload, and lucky for her patient, this speech-language pathologist (SLP) is always ready to learn about innovative ways to improve treatment for dysphagia. Meet Taylor Kae Hahn, owner of Maumee Bay Mobile Speech Services and dysphagia specialist.
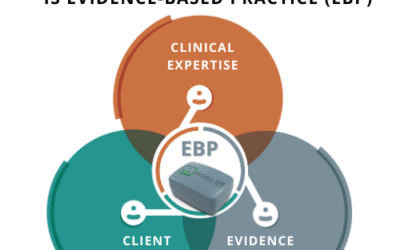
Taylor contacted us with a success story that we had to share as it truly highlights how the Mobili-T system works as an evidence-based, innovative solution for dysphagia therapy.
The impact of dysphagia
Taylor’s patient came to her after many years of living with a disordered swallow. She coughed frequently, had difficulty moving food and liquid back, and initiating a swallow. All this difficulty meant she often drooled as she could not effectively swallow her own saliva. As many do, this patient had come up with some workarounds. She would hold food or liquid in her mouth for up to two minutes until she could initiate a swallow. Sometimes, she would push on her cheeks to send the liquid back or use her fingers to push food back and try to trigger a swallow. She wore long sleeves to frequently wipe away saliva. While they sometimes got the job done, dysphagia was having a major impact on her nutrition and quality of life.
How sEMG became part of the picture
Taylor started by ensuring her patient had a safe swallow. A modified barium swallow study (MBSS) revealed that she was not aspirating, but even getting that data was difficult as she could barely initiate a swallow. Taylor then decided to take a look with a fiberoptic endoscopic evaluation of swallowing (FEES) and to really up the ante, she put a Mobili-T device on the patient’s swallowing musculature to give her visual biofeedback about when she was engaging her muscles. This is when something really clicked.
The patient could SEE how she was engaging her muscles to initiate a swallow, and with that visual feedback, she could replicate it. Meanwhile, Taylor was amazed to see how accurately Mobili-T was taking data. Comparing what she saw via FEES and on the screen with the Mobili-T system – they aligned perfectly in terms of tracking swallows and muscle engagement. She described her amazement saying, “It just confirmed with my own two eyes that this little device you stick on your chin is actually doing what you think it is doing. It’s not giving you false data.”
FEES is a commonly used tool for assessment, but it’s not sustainable as a therapy tool. You can’t set a patient up to use FEES on their own. Imagine giving an endoscope to your patient to feed through their nasal passages every time they wanted visual biofeedback during swallowing exercises. Not exactly motivating (and not exactly possible considering the training needed to conduct a FEES assessment). This is where Mobili-T stole the show. “This little device you stick on your chin.” It was as easy as that for the patient to take charge of their therapy.
Sticking with the Program
Taylor’s patient continued to use the Mobili-T system three times a week, following the swallowing exercise program. She has seen incredible results in her progress through Mobili-T’s program. “She loves it. She’s learning the form and realizing what she needs to do to get those faster swallows. And we’re getting to the point now where almost every box [on the screen] is filled.”
Outside of the exercises and therapy, this has translated into a much more prompt and effective swallow. “She can put a straw in her mouth and just swallow three swallows in a row without coughing,” Taylor describes. Taylor also reported her patient no longer needs to wipe her mouth constantly as she is able to swallow her own saliva.
Why Mobili-T Worked
While there is research detailing how the principles of motor learning apply to swallowing rehab (in short, to improve the swallow, therapy must focus on performing that swallow), Taylor realized how Mobili-T’s sEMG biofeedback helped this become a possibility:
“It’s the ability to SEE. It’s to be able to see when you are actually swallowing. To see the mind-body connection. It’s like her mind and her throat were just not connected until she could visualize what her swallow was doing.”
Taylor is looking forward to continuing to use Mobili-T on a variety of patients. “It’s really easy and universal to use. It’s compact and noninvasive. It’s not intimidating to patients. I would use it with any population.”
The Future of Dysphagia Therapy
Compensatory strategies and diet modification have historically been a huge part of dysphagia management. They do not alter swallowing function but compensate for the deficits. Taylor places a big emphasis of her practice on thinking outside these options to ways that she can help patients make progress towards improvement.
“It has been revolutionary for these clients that have had no idea how to change the biomechanics of their swallow and have just been compensating in these wild ways. I really think it’s important for more therapists to learn about dysphagia and therapy and to get rid of the old things that we’ve been doing that are just not helping clients.”
It’s working with innovative therapists like Taylor, and her patients that keep us striving towards improving outcomes using technology like the Mobili-T system. Thank-you to Taylor Kae Hahn for sharing her story!
If this story inspired you to try out some new tools in your facility, check out the case study version that you can share with your admin to get them on board with Mobili-T.