Understanding sEMG biofeedback signal for dysphagia: From brain signals to swallowing muscles to your phone screen
If you have a swallowing disorder (dysphagia), you may have seen a speech-language pathologist (SLP). The SLP may have given you some exercises to complete in the clinic and at home. The SLP may have even used a technology called sEMG biofeedback to help you “see your swallow”. During the exercise, you likely saw the biofeedback line go up as you swallowed and watched it return to a flat line once you were done. This biofeedback line helped you understand the exercise, but how did it actually represent your swallow?
(If you’ve never used biofeedback and wonder what it is, please read this short article or the little refresher below.)
What is sEMG
sEMG stands for surface (s) electro (E) myo (M) graphy (G). It is a visual representation of muscle activity. This muscle activity is captured by small sensors (the size of small buttons) that stick on the skin like stickers. Most patients with dysphagia do not have access to this type of technology.
Until now, sEMG has only been available for patients with dysphagia to use in select clinics. Mobili-T® allows you to take advantage of this technology from the comfort of your own home.
sEMG biofeedback is an established technology used with patients with swallowing disorders (dysphagia). To learn more read our article about exercises for swallowing disorders.
Is sEMG safe?
Yes.
This is a completely non-invasive technology. Surface electromyography (sEMG) sensors are placed right on the skin, like stickers. This feels like a piece of tape. The Mobili-T device does not do anything to you. You won’t feel anything from the system except that it is touching your skin.
Why does the sEMG sensor go under my chin?
To understand how swallowing function can be “seen” using surface electromyography (sEMG), we will first review the swallow. A typical, healthy swallow happens quickly, but it is extremely complex. There are about 30 pairs of muscles and 6 cranial nerves involved to make sure the food you eat makes it safely and quickly to your stomach.
The act of swallowing is a continuous sequence of movements that are typically described as 4 phases. These phases happen one after the other. They are:
- The oral preparatory phase (happens in the mouth)
- The oral transport phase (happens between the mouth and throat)
- The pharyngeal phase, and (happens in the throat)
- The esophageal phase (happens as the food makes its way to the stomach).
(For an in-depth, academic overview of the swallow, we recommend reading The Normal Swallow: Muscular and Neurophysiological Control by Stephanie Shaw and Rosemary Martino.)
The pharyngeal phase is the most complex of the four1. This phase includes an important starting event that keeps your swallow safe: a group of muscles contract. This contraction starts a chain reaction that positions your tongue, voice box, and throat in the best configuration for food to pass safely. This means it doesn’t go into your lungs. For anyone curious, these muscles include the mylohyoid, geniohyoid, anterior belly of the digastric, posterior digastric and the stylohyoid.
Three of these muscles (the mylohyoid, geniohyoid and anterior digastric) are found under the chin. Why is this important? Well, that is exactly where the sEMG sensors are typically placed2,3. In other words, we want to monitor when these muscles contract, how much they contract, and for how long. These muscles are the main contributors to sEMG signal collected under the chin4, although you may get some signal (called cross-talk)5.
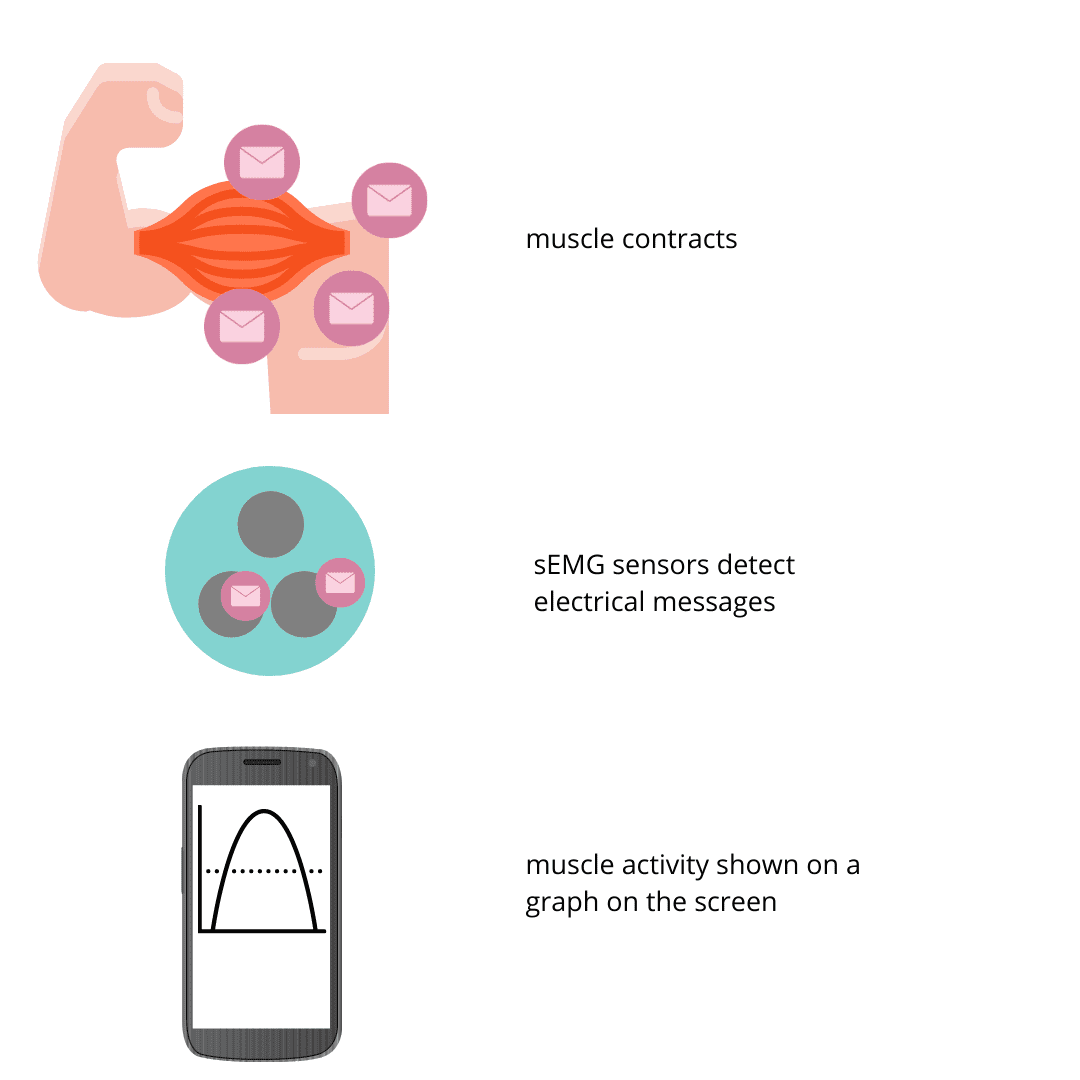
What happens between the brain and the muscle contraction?
When you move, your brain sends off a series of commands that go down the spinal cord and out over nerves to muscles. Muscles do what the brain tells them to do. When you think to yourself “I want to complete an effortful swallow now”, this message to contract your muscles is sent from the outer layer of the brain (cerebral cortex) to the relay centers in the part of your brain just above your spinal cord (motor nuclei of the cranial nerves). This message travels through a “cable” (corticobulbar tract) to the muscles under your chin.
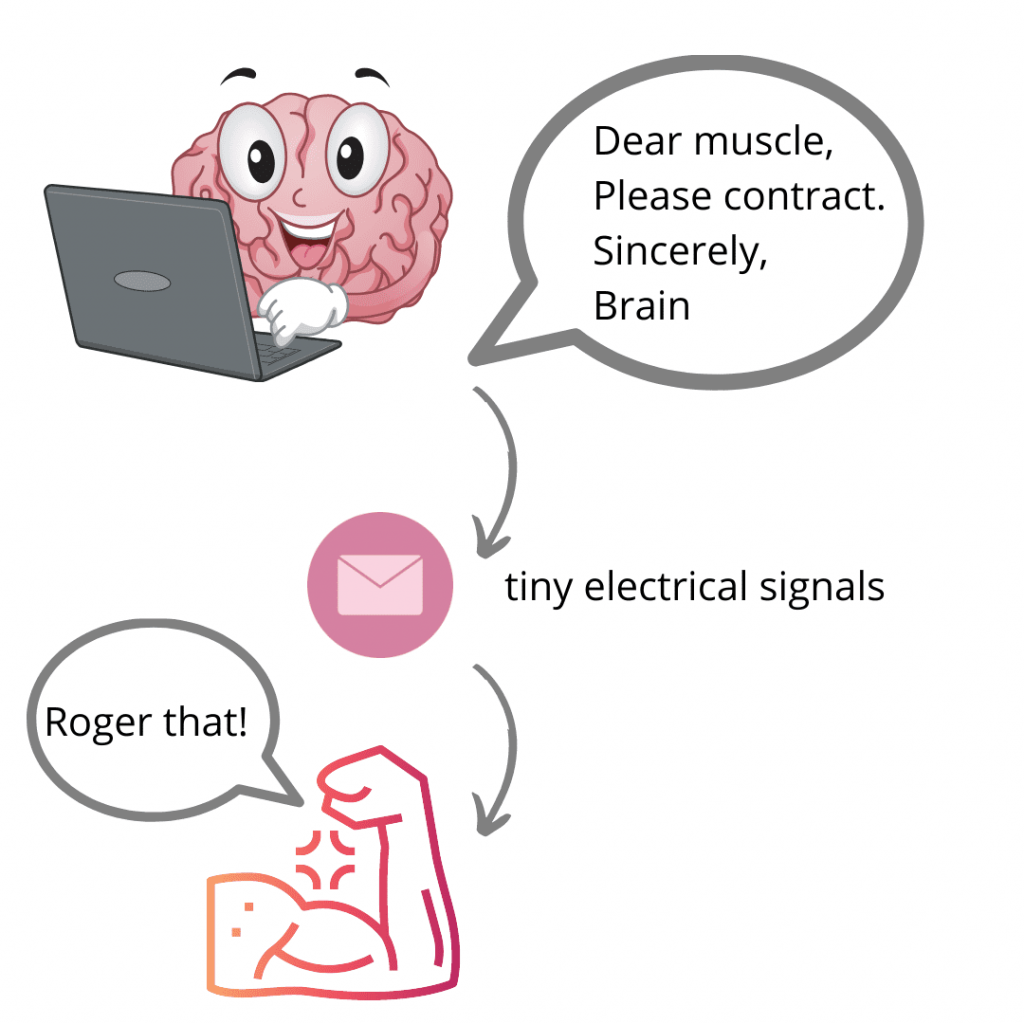
How do sEMG sensors detect muscle contraction messages?
We’ve used the term “message” above, but what we really mean are tiny electrical signals – your body activates muscles with its own electrical system! These tiny electrical signals are called action potentials. Think of these tiny electrical signals as emails that go from the CEO (the brain) to the workers (the muscles).
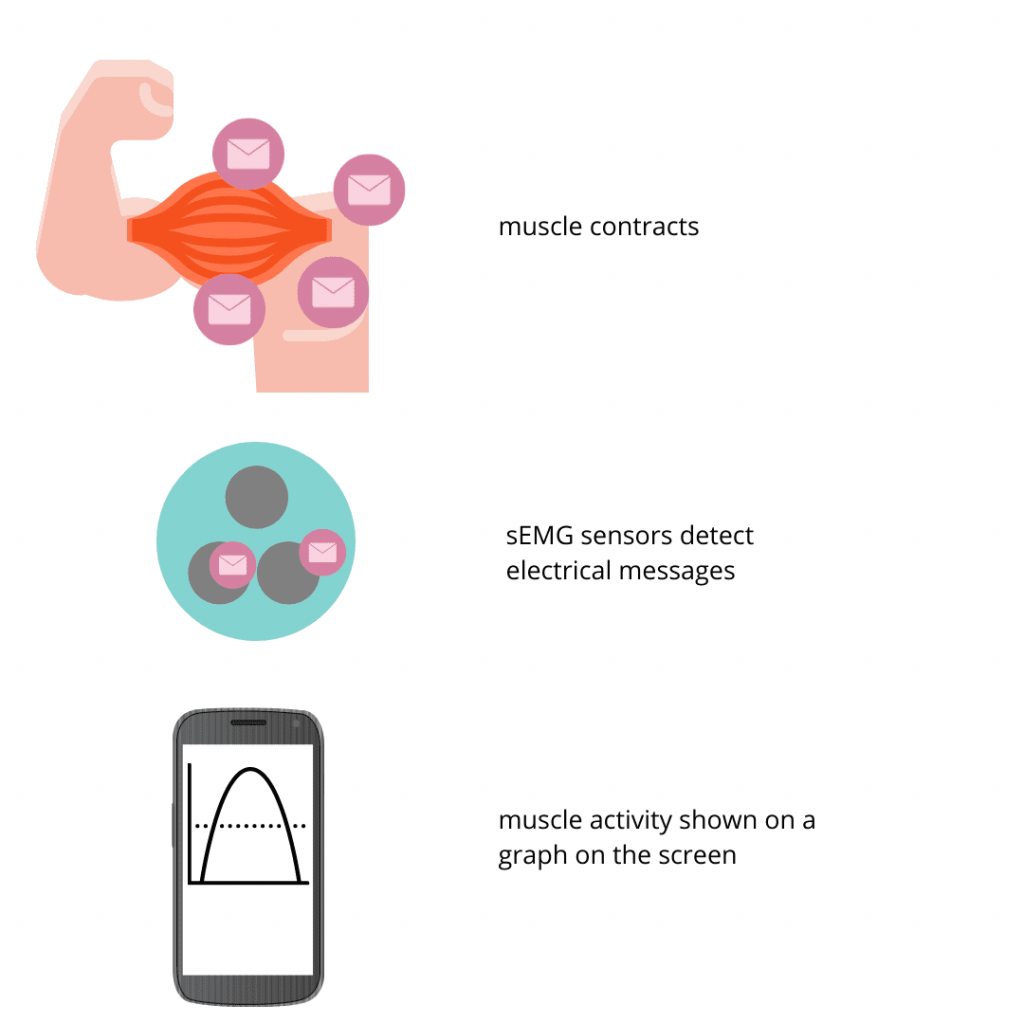
The sEMG sensors that are placed under your chin during exercise with biofeedback detect these electrical signals. The sEMG sensor can pick them up through your skin. sEMG sensors measure your body’s own electrical signals as they spread from one nerve over the surface of the muscle. The sensors detect how strong your body’s signals are and shows them on a screen so we can see how well the muscles are activated. sEMG is very sensitive and can pick up low levels of muscle activity that you may not even be able to feel.
What happens from the sensor to my phone screen?
The sEMG signal recorded from the muscles then goes through slight modifications. First, it is amplified (made bigger) so that it can be seen. It is also filtered to remove or reduce electrical noise and movement artifacts9. The signal is further modified so that it can be easily interpreted by you and your clinician. The resulting sEMG signal shape can be used by clinicians to monitor muscle activity.
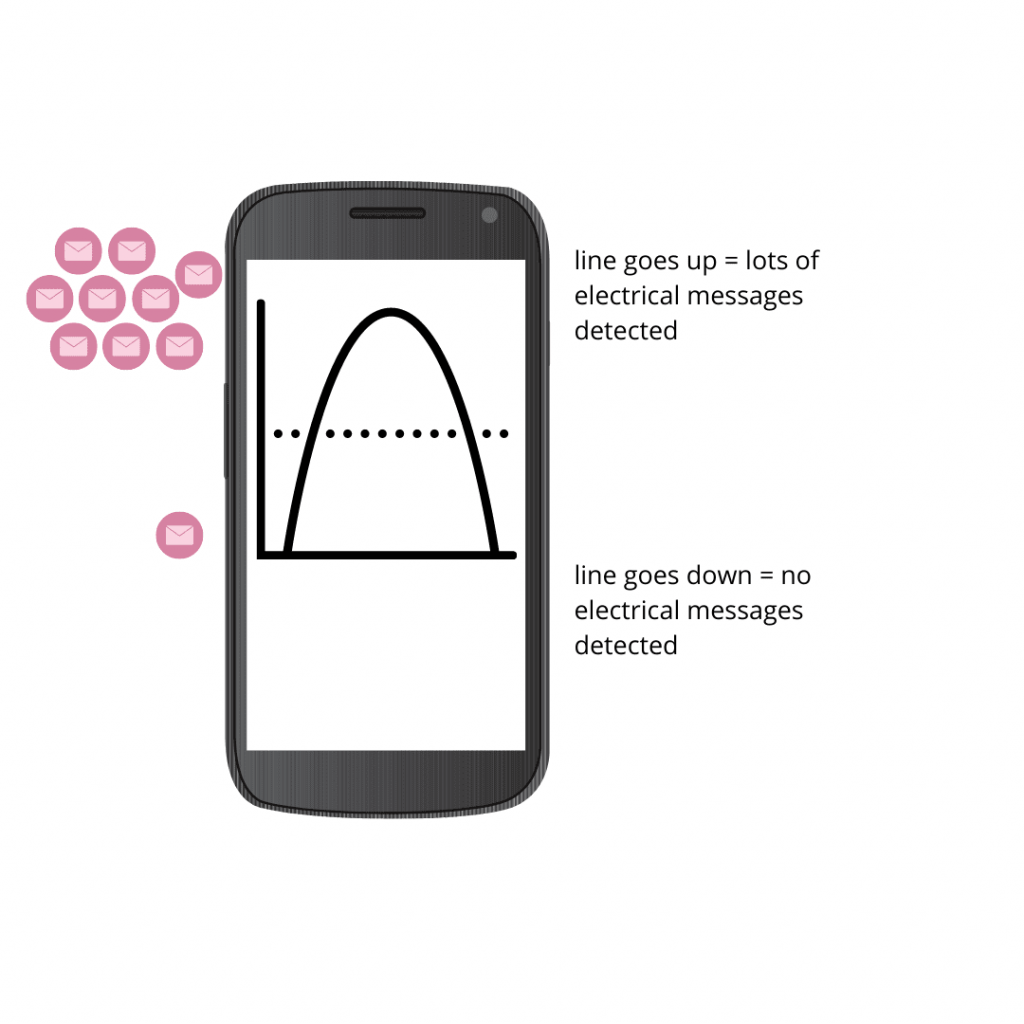
The sEMG biofeedback signal you see on your phone is a graph of voltage (μV) against time (s). A muscle contraction can be seen as an increase in signal height (line goes up). Muscle relaxation is seen as a return of the signal to baseline (line goes down). The height of the signal is related to the force of the contraction. The sEMG device measures voltage, which represents the relative level of muscle recruitment, not force.
How sEMG transforms dysphagia exercise
Unless you have biofeedback, there is no way to really know whether or not you are actually putting in more effort for that effortful swallow. There is also no way of really knowing if you are still holding that contraction for the Mendelsohn maneuver. Without the help of biofeedback, you are working in the dark. Using sEMG systems can take the guesswork out of swallowing exercises. By watching the biofeedback on the screen, you’ll be able to have a better sense of how your muscles are being activated.
Information that you and clinicians are typically interested in include: time when line went up (muscle onset), time when line went down (muscle offset), the length of time the signal stayed up (duration between onset and offset) and the average height of the signal (mean amplitude). This information can be used during swallowing therapy to detect achievements relevant to set targets3. In addition, calibration or normalization is used if wishing to track changes over time or make comparisons between individuals or between different swallow conditions3,9. This essentially means looking at a swallow muscle contraction relative to what would be a typical swallow for you. You wouldn’t want to compare your workout effort to those of a professional athlete.
We also encourage you to visit True Angle’s YouTube channel for three mini-tutorials on sEMG. These are free and accessible to anyone.
If you’ve enjoyed this article and want to learn more about other topics, or if you want to write a guest blog with us, send us a note at info@trueanglemedical.com