In the US alone, 1 in 6 adults reported difficulties with swallowing, or dysphagia1. The primary healthcare providers overseeing the management of dysphagia are speech-language pathologists (SLPs). An SLP can create a to help you manage your swallowing disorder. This plan may include changes in diet, techniques and postures that can help, and rehabilitation exercises. This article focuses on common rehabilitation exercises for the treatment of dysphagia.
Before we deep-dive, let’s figure out what exercise has to do with swallowing disorders.
Whether you are a fan of golf or absolutely despise the sport, we can all admire Tiger Woods’ golf swing. What is so fascinating about Mr. Woods is that he was able to adapt and re-train his muscular system after a serious back injury. So, you might be wondering what does Woods’ golf swing have to do with swallowing disorders or dysphagia?

- The golf swing requires coordination, timing and strength of several muscles including the arms, back and legs. This is like when you swallow. The muscles in your tongue, throat, and neck work together to transport food safely from your mouth to stomach.
- Human muscle systems are flexible and can adapt to new ways of functioning even after serious injuries. Dysphagia (swallowing disorders) may result from weakened or mis coordinated muscles. Dysphagia can also result from a change in the way your nervous system detects a safe swallow. Swallowing rehabilitation can help you adapt, maintain, and improve your swallowing muscular system.
- Just like Woods has a team of experts helping him to understand and treat his injury, you have a team of clinicians, researchers and entrepreneurs who are dedicated to helping you with your swallow.
Dysphagia or swallowing disorders can result from a number of different medical conditions. A qualified clinician will first diagnose *how* those conditions have impacted the swallow and *how* it can be improved. He or she will act as a detective and try to determine the cause of the swallowing difficulty. It could be due to muscle weakness, incoordination, altered anatomy in the mouth or neck, pain, dry mouth, fear, or a combination of all of these. Managing dysphagia is a top priority because swallowing impairments can have serious consequences on both physical and mental health.
What are the exercises shown to help with swallowing disorders and dysphagia?
Tiger Woods’ rehabilitation program was successful in part because of the rehabilitation exercise program that was tailored to areas he needed to work on: a combination of strength, endurance, and coordination. Similarly, your rehabilitation exercises will work best when tailored to your swallow. Your clinician may recommend exercises to help improve the strength, endurance, coordination/ timing of your swallow, or a combination of these. Two exercises that are often prescribed because they target most of these areas are:
- the Effortful Swallow. In this swallowing rehabilitation exercise, your clinician may ask you to “swallow as hard as you can” or “push really hard with your tongue as you swallow”. This exercise has been shown to
- improve the flow of food when you swallow
- reduce food left in your throat after you swallow
- improve the strength (pressure) of your swallow
- the Mendelsohn Maneuver. This exercise is a little trickier so your clinician may begin by first bringing your awareness to your regular swallow. Your clinician may ask you to put your finger on the Adam’s apple (thyroid notch). Then they will ask you to swallow. You should feel how your Adam’s apple goes up as you swallow, and comes back down at the end of your swallow. Once you notice this movement, your clinician will then ask you to perform this exercise: As your Adam’s apple goes up during the swallow, squeeze your throat muscles and hold for 2 to 5 seconds. You should feel your Adam’s apple stay up during that time. Over time, this exercise has been shown to:
- improve coordination and timing of the swallow
- reduce the amount of food going down the wrong way (aspiration)
Swallowing exercises are most helpful when they are practiced frequently, specific to a goal, and are challenging2.
- Practicing frequently: If we go back to Mr. Woods, he practices his golf swing daily to perfect his technique. Just like Mr. Woods, to improve a swallowing impairment, you too need to practice often. How often is often? It really depends on your goals, starting point and cause of swallowing difficulties. Your clinician will be able to help you determine how long and how often you should exercise.
- Specific to a goal: It wouldn’t make much sense if Mr. Woods played soccer as a way of practicing golf. When it comes to swallowing, you need to practice swallowing related exercises.
- Challenging: To perform a powerful golf swing, Mr. Woods needs to challenge his body. For example, he might set the goal of hitting the golf ball further and further every week. Similarly, in swallowing you need to push your muscles every time you practice. For example, if your exercises involve food, your clinician may ask you to eat something a bit more difficult than in your last exercise.
Clinicians use these principles and the best available evidence to guide swallowing rehabilitation. As new technology and exciting research emerges, clinicians consistently incorporate these new findings to provide their patients with the best quality of care. These new findings can strengthen what clinicians know or can provide guidance on how to improve treatment. We encourage you to ask your clinician questions about new evidence and technology.
Are swallowing exercises the only thing I can do to manage my dysphagia?
There are a number of approaches to ensure that someone swallows safely and efficiently. A qualified clinician, such as a speech-language pathologist, will be well versed in selecting these approaches and tailoring them to your needs.
Aside from rehabilitation exercises, dysphagia can be managed using:
- Compensatory techniques. For example, a clinician may recommend a thicker liquid that moves more slowly and is easier to swallow for some individuals. A clinician may also ask an individual to tuck in their chin to help with swallowing (e.g., chin tuck).
- Stimulatory techniques. For example, a clinician may recommend swallowing cold liquids to help you feel where the liquid is.
Although these additional techniques exist, swallowing rehabilitation exercises are still an essential part of a dysphagia management plan. Swallowing exercises may be recommended with the aim of preventing, improving, maintaining, or reducing decline of your swallow function over the long term.
How do I usually learn how to perform swallowing exercises with my clinician?
The way you learn how to perform exercises is different and depends on many factors, including the resources to which your clinician has access. Your clinician may use a combination of tools including verbal instruction, diagrams, mobile applications, and other technologies. For example, one of the instructions for Effortful Swallow is to “swallow hard”, but what does that mean?

Describing what to do with your swallowing muscles using verbal instruction and diagrams on paper can be difficult. This is because you cannot see what your swallowing muscles are doing in the same way that Mr. Woods can see his golf swing. Not only is it hard for you to understand, but it’s also hard for your clinician to describe as well.
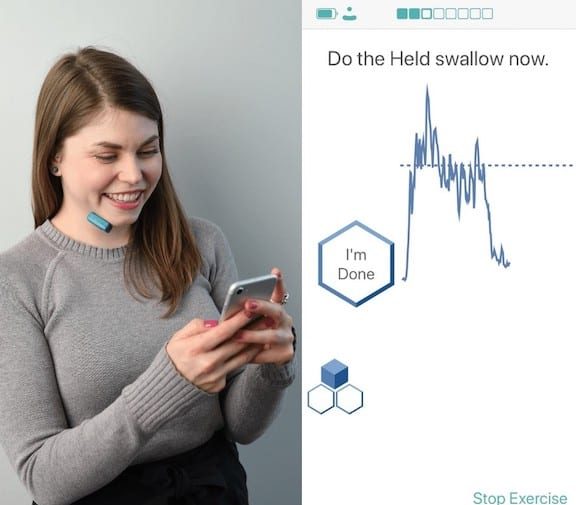
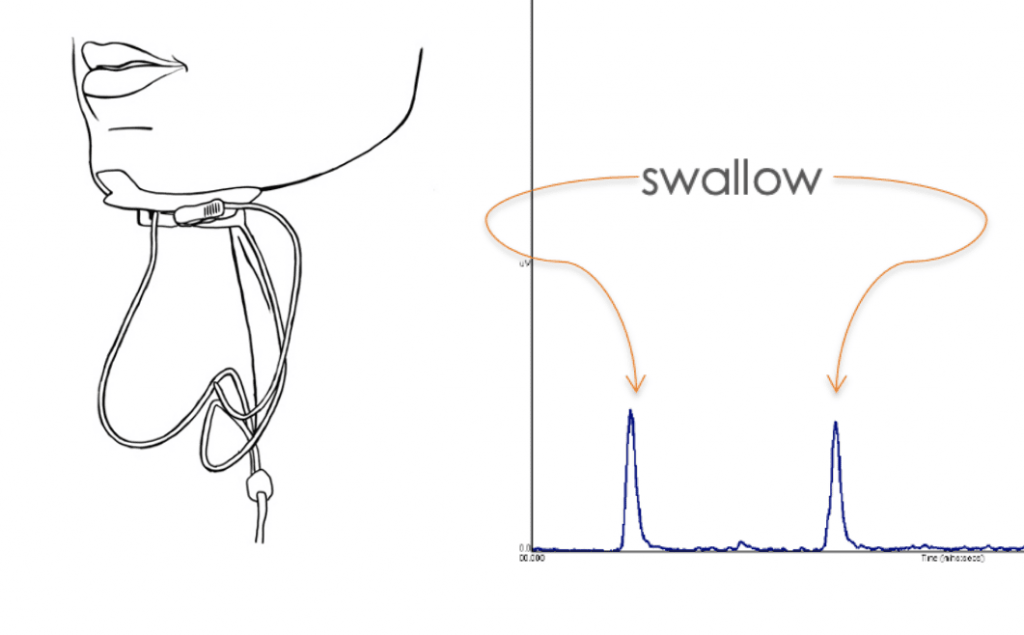
To get around this problem, some clinicians use biofeedback. Biofeedback is a way of monitoring information related to your body. In our case, we are trying to understand what your muscles are doing while you complete swallowing exercises. A type of biofeedback used in swallowing rehabilitation is surface electromyography (sEMG). Clinicians have used sEMG biofeedback to help with the learning of the Mendelsohn Maneuver and Effortful Swallow.
sEMG biofeedback works using these two key components3: 1) a way to sense or pick up signals from your muscles. This is done using sensors that stick to the underside of your chin; and 2) a way for you to see the signals from your muscles. This involves a way of collecting and graphing the activity of your muscles. In the clinic, this information is shown on a computer screen.
sEMG biofeedback has been around since the 70s. There is a lot of exciting new research supporting the benefit of using sEMG biofeedback to help with learning and getting the most out of your swallowing exercises. For example, in a study with individuals with stroke related dysphagia, researchers asked participants to practice swallowing exercises with and without sEMG biofeedback4. The researchers found that participants performed the exercises better when they used sEMG biofeedback. The participants said biofeedback helped them see what they were doing and helped their clinician coach them through the exercise. Not only has biofeedback been reported to help with exercise instructions, 14 studies with different populations (Parkinson’s, Stroke, Alzheimer’s, head and neck cancer and brain stem injury) have reported improvement in eating and drinking 5-17
But accessing sEMG biofeedback has been difficult:
- Typically this equipment can be as large as a fridge and is quite expensive.
- Some clinics do not have access because it’s too expensive and/or it is no longer manufactured.
- Individuals with swallowing exercises can’t take this machine home. Home is where the biggest bulk of swallowing exercise takes place.
Rehabilitation exercises are an important part of the management and treatment of dysphagia. Not only is it important to stick to a regular exercise routine, but you also set specific exercise goals and challenge your system. With the help of your speech-language pathologist and new technology, you can practice swallowing exercises from the comfort of your own home and keep up that routine!
About Mobili-T: Mobili-T is the innovative wireless sEMG biofeedback device that helps you live well with dysphagia.
References
- Adkins, C., Takakura, W., Spiegel, B. M., Lu, M., Vera-Llonch, M., Williams, J., & Almario, C. V. (2020). Prevalence and characteristics of dysphagia based on a population-based survey. Clinical Gastroenterology and Hepatology, 18(9), 1970-1979. pubmed.ncbi.nlm.nih.gov/31669055/
- Robbins, J., Butler, S. G., Daniels, S. K., Gross, R. D., Langmore, S., Lazarus, C. L., … & Rosenbek, J. (2008). Swallowing and dysphagia rehabilitation: translating principles of neural plasticity into clinically oriented evidence. Journal of Speech, Language, and Hearing Research. pubmed.ncbi.nlm.nih.gov/18230851/
- sEMG article on the National Foundation of Swallowing Disorders website: swallowingdisorderfoundation.com/swallowing-exercise-with-biofeedback/
- Archer, S. K., Smith, C. H., & Newham, D. J. (2020). Surface Electromyographic Biofeedback and the Effortful Swallow Exercise for Stroke‑Related Dysphagia and in Healthy Ageing. Dysphagia. pubmed.ncbi.nlm.nih.gov/32445060/
- Haynes, S. N. (1976). Electromyographic biofeedback treatment of a woman with chronic dysphagia. Biofeedback and Self-Regulation, 1(1), 121-126. pubmed.ncbi.nlm.nih.gov/990340/
- Bryant, M. (1991). Biofeedback in the treatment of a selected dysphagic patient. Dysphagia, 6(3), 140-144. pubmed.ncbi.nlm.nih.gov/1914542/
- Huckabee, M. L., & Cannito, M. P. (1999). Outcomes of swallowing rehabilitation in chronic brainstem dysphagia: a retrospective evaluation. Dysphagia, 14(2), 93-109. pubmed.ncbi.nlm.nih.gov/10028039/
- Crary, M. A., Carnaby, G. D., Groher, M. E., & Helseth, E. (2004). Functional benefits of dysphagia therapy using adjunctive sEMG biofeedback. Dysphagia, 19(3), 160-164. pubmed.ncbi.nlm.nih.gov/15383945/
- Bogaardt, H. C. A., Grolman, W., & Fokkens, W. J. (2009). The use of biofeedback in the treatment of chronic dysphagia in stroke patients. Folia Phoniatrica et Logopaedica, 61(4), 200-205. pubmed.ncbi.nlm.nih.gov/19590219/
- Carnaby-Mann, G. D., & Crary, M. A. (2010). McNeill dysphagia therapy program: a case-control study. Archives of physical medicine and rehabilitation, 91(5), 743-749. pubmed.ncbi.nlm.nih.gov/20434612/
- Carnaby-Mann, G., & Crary, M. (2009, December). A case-control evaluation of the McNeill dysphagia therapy program (MDTP). In Dysphagia (Vol. 24, No. 4, pp. 451-451). 233 SPRING ST, NEW YORK, NY 10013 USA: SPRINGER.
- McCullough, G. H., Kamarunas, E., Mann, G. C., Schmidley, J. W., Robbins, J. A., & Crary, M. A. (2012). Effects of Mendelsohn maneuver on measures of swallowing duration post stroke. Topics in stroke rehabilitation, 19(3), 234-243. pubmed.ncbi.nlm.nih.gov/22668678/
- McCullough, G. H., & Kim, Y. (2013). Effects of the Mendelsohn maneuver on extent of hyoid movement and UES opening post-stroke. Dysphagia, 28(4), 511-519. pubmed.ncbi.nlm.nih.gov/23494471/
- Steele, C. M., Bennett, J. W., Chapman-Jay, S., Cliffe Polacco, R., Molfenter, S. M., & Oshalla, M. (2012). Electromyography as a biofeedback tool for rehabilitating swallowing muscle function. Applications of EMG in clinical and sports medicine, 311-328.
- Athukorala, R. P., Jones, R. D., Sella, O., & Huckabee, M. L. (2014). Skill training for swallowing rehabilitation in patients with Parkinson’s disease. Archives of Physical Medicine and Rehabilitation, 95(7), 1374-1382. pubmed.ncbi.nlm.nih.gov/24816250/
- Tang, Y., Lin, X., Lin, X. J., Zheng, W., Zheng, Z. K., Lin, Z. M., & Chen, J. H. (2017). Therapeutic efficacy of neuromuscular electrical stimulation and electromyographic biofeedback on Alzheimer’s disease patients with dysphagia. Medicine, 96(36). pubmed.ncbi.nlm.nih.gov/28885365/
- Azola, A. M., Sunday, K. L., & Humbert, I. A. (2017). Kinematic visual biofeedback improves accuracy of learning a swallowing maneuver and accuracy of clinician cues during training. Dysphagia, 32(1), 115-122. pubmed.ncbi.nlm.nih.gov/27677733/