Habilitation vs. Rehabilitation
Dysphagia in adults can look very different from pediatric dysphagia (i.e., swallowing disorders in infants or children). One of the major differences between the two groups is the cause or etiology of dysphagia. Most cases of dysphagia in adults are acquired. This means that the individual previously had a typical or healthy swallowing function, but due to medical circumstances such as stroke, dementia, or traumatic brain injury, is now experiencing dysphagia (Groher & Crary, 2016). In contrast, most cases of dysphagia in infants or children are congenital, meaning that feeding and swallowing difficulties are present at birth (Rebecca Perlin, personal communication, March 25, 2022).
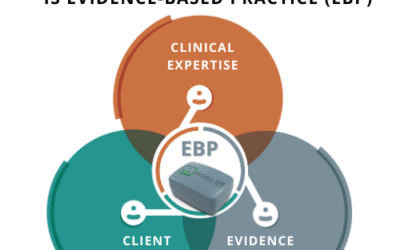
The differences in the cause of dysphagia between adults and infants or children also lead to differences in the approach to assessment and treatment. Because adults with dysphagia have most likely experienced the loss of previous abilities, assessment and treatment of their swallowing difficulties often strives for a rehabilitative approach (Smith, et al., 2012). This means that treatment will likely involve strategies that will help adults with dysphagia restore (or maintain) the function they have lost. One example of these rehabilitative approaches for adults with dysphagia is using intensive exercises to regain the coordination and strength necessary for swallowing. Speech-Language Pathologist and Newborn Individualized Developmental Care and Assessment Program (NIDCAP) professional, Julia Giesen, shares that unlike services for adults with dysphagia, your child’s healthcare team will most likely use a habilitation approach (Julia Giesen, personal communication, March 23, 2022). This means that treatment will involve building a new system (i.e., feeding) from the ground up, starting with ensuring that foundational skills are practiced and achieved. For example, before a child can work on eating solid foods, they first need to achieve voluntary mouth movement. In this example, the transition from reflexive mouth movement, such as when an infant suckles on a nipple, to voluntary mouth movement, such as when a child is chewing solid food, is an important foundational step needed to build that feeding system.
The Zone of Proximal Development and Pediatric Dysphagia

According to Dr. Giesen, “Many pediatric patients demonstrate slower or disrupted development […] to manage and manipulate food in the mouth and coordinate the swallow” (personal communication, March 23, 2022). Because of this, you may find that your child’s feeding and swallowing abilities do not match that of their peers. Even though your child can progress and improve their feeding and swallowing abilities through treatment, it is likely that your child may continue to display differences when compared to other children their age.
This is okay.
During treatment, your child’s health care team will work towards goals that are within your child’s ‘zone of proximal development’ (ZPD). The ZPD is defined by the difference between what a person can do on their own and what they can do with support. Working in a child’s ZPD means working on skills that are just beyond their current abilities, or in other words, what they are able to do with support. For example, if your child was learning to walk and using the couch to balance, a skill that would be within their ZPD would be walking a few steps while holding onto one of your fingers. What is important about your child’s ZPD is that it is unique to them. It is not dependent on age or typical development, but rather it is dependent on the skills that your child can currently achieve with support. This is why it is important to try to resist the natural tendency to compare your children’s abilities to other children their age. However tempting it may be to compare your child to their peers, know that wherever your child is at in their development, it is okay. Your child’s healthcare team will work with you to do everything possible to support your child’s feeding and swallowing progress at your child’s own pace.
Supporting Your Child Where They Are

Knowing that your child has their healthcare team to support them hopefully gives you some peace of mind, but you may also be left wondering where you, the parent, fit into the picture. A study conducted in 2020 showed that parents and caregivers want to be involved in the assessment and treatment planning for their child (Simione, et al., 2020), but it is not uncommon that parents are left wondering, What canI do to support my child’s feeding and swallowing? The answer to this question is not “one size fits all” as your involvement in your child’s dysphagia treatment or management is dependent on a number of factors. Some of these factors include the cause of your child’s dysphagia, their treatment plan, or the presence of any other medical conditions. Your healthcare team will be able to discuss different ways you can best support your child’s feeding and swallowing and help you feel involved.
What you can know for certain, however, is that whatever you are doing is enough. Children experiencing dysphagia often have additional medical needs, and this is something that can weigh heavily on a parent. Healthcare professionals may ask you to report on your child’s symptoms, answer seemingly endless questions, attend all of their appointments, and possibly carry out treatment activities at home as well. This is a lot, and the advocacy, support, and love you continuously give your child does not go unnoticed. So when asking, What can I do to support my child’s feeding and swallowing?, know that accepting and loving your child wherever they are at developmentally is enough.
References
- Groher, M. E., & Crary, M. A. (2016). Dysphagia: Clinical management in adults and children. Elsevier.
- Simione, M., Dartley, A. N., Cooper-Vince, C., Martin, V., Hartnick, C., Taveras, E. M., & Fiechtner, L. (2020). Family-centered outcomes that matter most to parents: A pediatric feeding disorders qualitative study. Journal of Pediatric Gastroenterology and Nutrition, 71(2), 270–275. https://pubmed.ncbi.nlm.nih.gov/32304556/
- Smith, S. K., Roddam, H., & Sheldrick, H. (2012). Rehabilitation or compensation: time for a fresh perspective on speech and language therapy for dysphagia and Parkinson’s disease? International Journal of Language & Communication Disorders, 47(4), 351–364. https://pubmed.ncbi.nlm.nih.gov/22788222/
- Yetman, D. (2020). What is the zone of proximal development? Healthline. https://www.healthline.com/health/zone-of-proximal-development